Providing safer, more accommodating health care for adults with autism
A specialized team at Ohio State delivers primary care designed for young adults on the autism spectrum
James Shannon knows he’s special. A silver medal hangs in his bedroom from the 2022 USA Special Olympics in which “Cannon Shannon,” as his coach calls him, helped the soccer team secure a spot on the podium with the two goals he scored in the national competition held that year in Florida.
But it’s more than soccer prowess that makes Shannon feel special. As a person on the autism spectrum, Shannon is an advocate for himself and others whose brains function differently in communication, information processing and sensory sensitivity.
“It’s not bad to be different,” Shannon says.
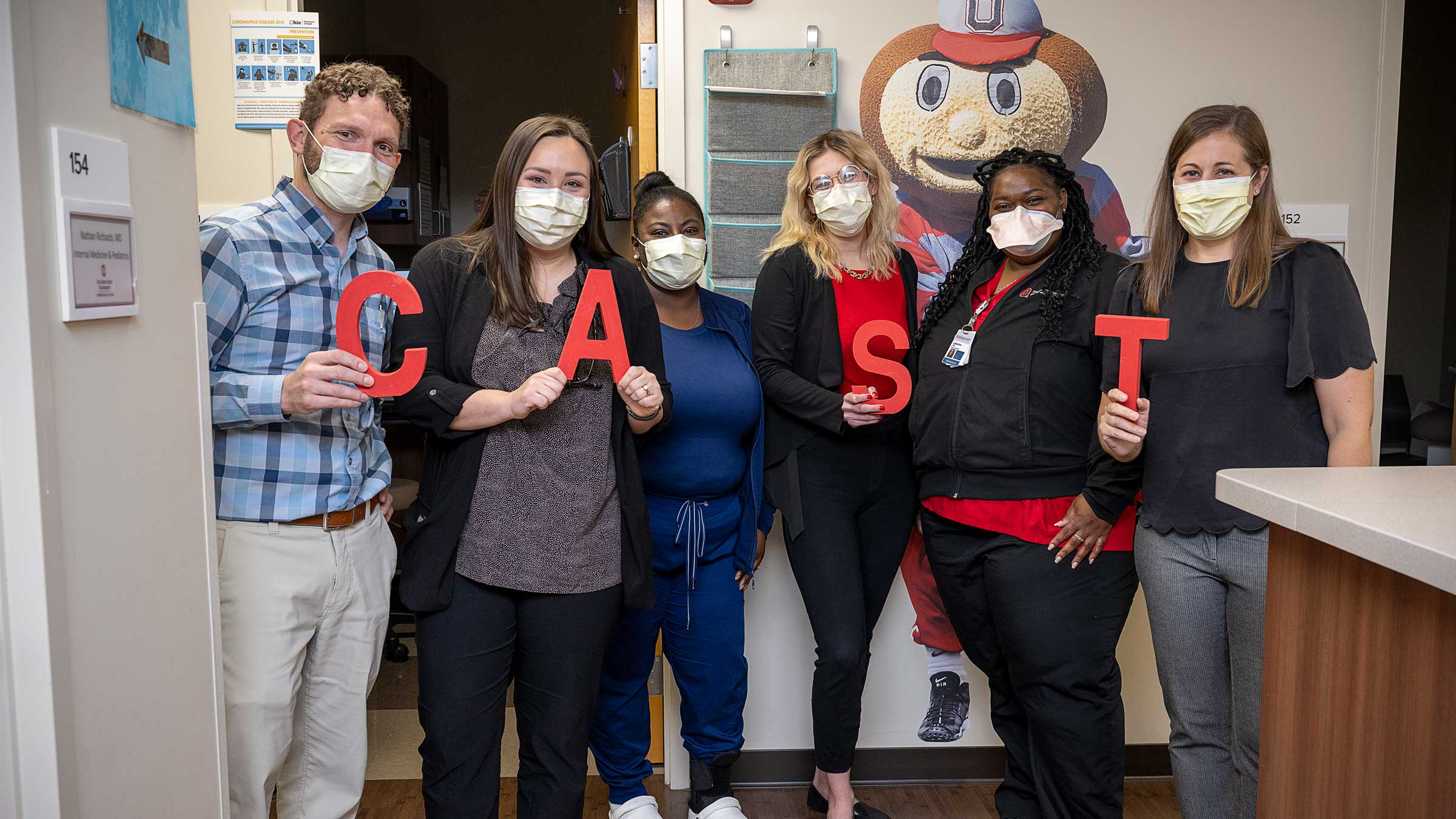
That message is one Shannon hopes will reach more health care providers. It’s the reason he chooses to receive his primary medical care from a team of clinicians at The Center for Autism Services and Transition (CAST), Ohio State’s primary care clinic for young adult patients 18 and older on the autism spectrum.
Now 25, Shannon began attending CAST around 2019 when his general practice physician retired. He liked the idea of seeing providers who understand autism and value people on the autism spectrum. Shannon believes clinics like CAST are critical to helping teens transition into adulthood.
“Some kids don’t feel special and feel like they don’t belong,” Shannon says. “And I feel like I don’t want doctors and health care persons to not include people with autism and push them away. Doctors need to know more.”
Grassroots origins and national model for adults with autism
CAST was created in 2014 in response to families of adult children on the autism spectrum seeking safer, more accommodating health care services than what they were experiencing in general clinical settings.
Those families provided input that shaped the innovative approach that CAST continues to offer to a growing population of patients as they age out of pediatric care. Bill and Marci Ingram, who support autism research and care at The Ohio State University, provided the clinic’s start-up funding and remain integral to CAST’s success.
During its eight years in operation, CAST has treated more than 1,000 patients and become a national model for other providers. Its research-based approach provides a blueprint for general-practice providers treating patients on the autism spectrum as well as next-generation specialty clinics.
In central Ohio, CAST guided Boundless, a nonprofit organization providing support services for people of all ages with intellectual and developmental disabilities, in developing a health care clinic that opened in September 2022.
“Because we have enough patients and I’ve been able to team up with good researchers, we can show that we have improved care, we have better preventive care rates and we have lower ER visit rates than the overall United States population of autistic individuals,” says Christopher Hanks, MD, CAST’s founding medical director and a clinical associate professor of Internal Medicine at The Ohio State University College of Medicine. “So, we share our approaches.”
Flexible, patient-centered care for young adults with autism
Shannon, who describes himself as shy, says he had reservations about his initial visit to CAST at age 22. “I was nervous the first time because I was going to meet new doctors and new people.”
Dr. Hanks put Shannon at ease, and before long Shannon was making jokes and forgetting about his nerves. “I made fun of his name because of the actor (Tom Hanks),” Shannon says.
Dr. Hanks believes accommodating different communication needs is essential to ensuring that patients receive optimal care. A patient who communicates better in writing, for instance, will come to an appointment with a written list of what they want to address for the provider to read.
“Health care is very much about communication,” Dr. Hanks says. “We know that a core feature of autism is that there are frequently differences in communication. That may be that the individual struggles with communication. Or, it may be that they communicate very well, but when they feel overwhelmed or stressed by sensory experiences, they struggle to communicate at their best.”
Because exams can create anxiety for people on the autism spectrum, CAST gives patients opportunities to prepare for appointments in advance. This modification helps to decondition patients from past negative health care experiences and shortens examination times.
“A blood draw is our most common example,” Dr. Hanks says. “You don’t have to have autism to dread getting your blood drawn. But if you’ve been held down in the past or forcefully had a blood draw or vaccine, then the next time that’s done, that’s going to be hard.”
CAST’s “happy visits” give patients the option to visit the clinic before a scheduled appointment. CAST also created videos for patients, which they are encouraged to watch and then role-play with family members before their exam.
Driven by a need for health care for autistic patients
From 2000 to 2018, the number of children diagnosed on the autism spectrum increased from 1 in 150 to 1 in 44, according to the Centers for Disease Control.
Today, adults on the autism spectrum account for an estimated 2% of the population, or close to 20,000 people in central Ohio.
“The need is massive. We can’t keep up with the demand,” Dr. Hanks says.
CAST remains one of the nation’s largest clinics — if not the largest clinic — dedicated to treating adults on the autism spectrum, Dr. Hanks says. CAST has accommodated an average of 10 new patients each month over its eight years. It currently treats about 650 active patients at its two clinics in the Columbus suburbs of Hilliard and New Albany.
Extending CAST’s reach to general practitioners
With so many patients in need of service, CAST provides education and support of general-practice providers to expand options for adult patients on the autism spectrum within the broader health care community.
Close to 100 Ohio State College of Medicine residents and medical students have spent time with CAST patients to gain practical experience in providing care to this population. Ohio State has a grant to develop training modules for residents with the goal of producing more primary-care and adult-specialty physicians who will care for adult patients on the autism spectrum.

“It’s very clear that physicians don’t feel like they know enough to care for this population,” says Dr. Hanks, who is integral to the Ohio State research team led by Brittany Hand, PhD, OTR/L, an assistant professor in Ohio State’s School of Health and Rehabilitation Sciences, developing the training modules.
When CAST was founded, none of its staff had experience working with patients on the autism spectrum. Having been there themselves, they understand their colleagues’ trepidation.
To provide support, CAST staff offer electronic consults and developed video trainings for general practitioners showing CAST’s techniques for exam procedures that can trigger patients, namely blood draws, electrocardiograms and blood pressure tests. The blood-draw video has been viewed 16,000 times.
Safety net for a vulnerable population
Since the COVID-19 quarantine periods, Shannon says he has struggled to emerge from the cocoon of his parents’ house in the Columbus suburb of Dublin. Besides participating in Special Olympics, his main outlet is taking classes at a community college.
Even without the added burden of the pandemic, the isolation Shannon describes is common for adults on the autism spectrum as they reach what is called “the services cliff” of young adulthood.
People on the autism spectrum lose access to resources between ages 18 and 22. Services such as occupational therapy and psychology, which help them integrate into the community, end when they complete secondary school. At age 22, they’re no longer entitled to services under the Individuals with Disabilities Education Act.
“They go from having a lot of support to having nothing,” Dr. Hanks says. “And, as we know, health is impacted by a lot of other things in life. Adults on the autism spectrum tend to be under-employed, under-socialized, under-insured. Those are big drivers for obesity and other health conditions.”
CAST provides a critical safety net for this vulnerable population by addressing common conditions of sleeping difficulty, gastrointestinal problems, weight control, behavioral health and more.
Increasing preventive care for autistic adults
“Preventive care is especially important for this population because they’re at higher risk than the general population for mental and physical health conditions that can be detected, prevented or managed with routine care,” says Dr. Hand.
Dr. Hand is highly regarded for her expertise and research in health service delivery and patient health outcomes among adults on the autism spectrum.
In 2021, Dr. Hand led a study published in the Journal of General Internal Medicine comparing 490 CAST patients from Ohio to 980 Medicare patients with autism and 980 privately insured patients with autism nationwide.
“We found that CAST patients had significantly greater odds of receiving any preventive service than Medicare-enrolled and privately insured adults with autism,” Dr. Hand says. “CAST patients were also significantly more likely to receive screenings and vaccinations than the national groups of adults with autism with private insurance or Medicare.”
Small steps bridge the gap for autistic adults
Dr. Hanks and Dr. Hand both see the extraordinary need to expand health care services for adults on the autism spectrum.
“With a population as large as this, we have to incorporate them into our regular health care system,” Dr. Hanks says. “This isn’t hard. What we’ve done at CAST is we’ve listened to our patients and made little tweaks for them, and that’s all it took to bridge this gap. You just have to meet patients where they are.”
In Shannon’s words: “If doctors knew more about us, we would have more places that would include people with autism and figure out what we need medically.”

Specialized care for young adults on the autism spectrum
The Ohio State Center for Autism Services and Transition (CAST)
Learn more





